Support Our Efforts
Prenatal-onset GBS
Disease Prevention
Also on this page: Membrane Stripping & Preterm Labor
View our past Symposium on POGBSD
View our past Symposium on POGBSD
Prenatal-onset GBS (POGBS) Disease includes miscarriages and stillbirths caused by group B strep. Currently, babies who are born already infected with group B strep are classified as "early-onset" regardless of when the infection began. According to a 2012 study done by Tudela and colleagues, "We hypothesize that these data support the concept that early-onset GBS represents a spectrum of infection that often precedes birth." |
GBSI advocates that the timing of when the infection began should determine if a baby had early-onset vs. prenatal-onset GBS disease. This is important as early-onset prevention strategies don't prevent GBS infections beginning before a woman's labor starts or her water breaks. In looking at individual cases, did the early-onset strategy fail or could something different have been done to protect a particular baby?
Please view Defining Prenatal-onset Group B Strep Disease (POGBSD) for further information.
Healthcare providers: Please view Table 1 of Development of Putative Working Definitions of Prenatal-onset Group B Strep (POGBS) Invasive Disease for proposed working definitions for POGBSD.
According to the CDC 2010 MMWR, "The burden of prenatal-onset GBS disease has not been assessed adequately and no effective prevention tools have been identified before the intrapartum period." However, a 2015 study estimated that 57,000 fetal infections/stillbirths occur annually. A separate systematic review in 2015 found that up to 12.1% of stillbirths are caused by GBS, noting that more research is needed. (12.1% of the World Health Organization's estimate of 2.6 million stillbirths per year suggests that 314,600 stillbirths may be caused by GBS, contrary to the the common thought that GBS-caused stillbirths are rare.)
Although there are no official guidelines regarding prenatal-onset GBS disease prevention, following are several knowledge-based strategies which may help prevent unborn babies becoming infected by group B strep or other harmful microorganisms:
Please view Defining Prenatal-onset Group B Strep Disease (POGBSD) for further information.
Healthcare providers: Please view Table 1 of Development of Putative Working Definitions of Prenatal-onset Group B Strep (POGBS) Invasive Disease for proposed working definitions for POGBSD.
According to the CDC 2010 MMWR, "The burden of prenatal-onset GBS disease has not been assessed adequately and no effective prevention tools have been identified before the intrapartum period." However, a 2015 study estimated that 57,000 fetal infections/stillbirths occur annually. A separate systematic review in 2015 found that up to 12.1% of stillbirths are caused by GBS, noting that more research is needed. (12.1% of the World Health Organization's estimate of 2.6 million stillbirths per year suggests that 314,600 stillbirths may be caused by GBS, contrary to the the common thought that GBS-caused stillbirths are rare.)
Although there are no official guidelines regarding prenatal-onset GBS disease prevention, following are several knowledge-based strategies which may help prevent unborn babies becoming infected by group B strep or other harmful microorganisms:

1) Urine culturing for GBS and other bacteria
In the US, this is usually done at the first prenatal visit and is different than the standard prenatal urine “dipstick” check. The American College of Obstetricians and Gynecologists (ACOG) issued new guidance in 2019 regarding Bacteriuria (GBS in urine) in regards to early-onset disease prevention. However, studies have shown that treating asymptomatic bacteriuria can reduce the risks of preterm birth. Further research is needed to see if perhaps urine culturing can also provide opportunities to reduce the risk of GBS infection for unborn babies.
Urine culturing is important because having GBS in your urine means that you are likely to be heavily colonized vaginally where GBS could potentially harm your baby. You may have GBS in your urine without having any symptoms, but see your provider promptly if you do have any symptoms of a bladder (urinary tract) infection.
Ask about the results of your urine culture:
2) See your provider promptly for an exam if you have any “vaginitis” symptoms
GBS can cause vaginitis symptoms such as:
These symptoms may be mistaken for a yeast infection and treated incorrectly.
Healthcare providers: Please view the poster presentation, Revisiting group B strep (GBS) symptomatic vaginitis (GBSSV), for more information.
View studies about Vaginitis & GBS
3) Avoid unnecessary invasive procedures
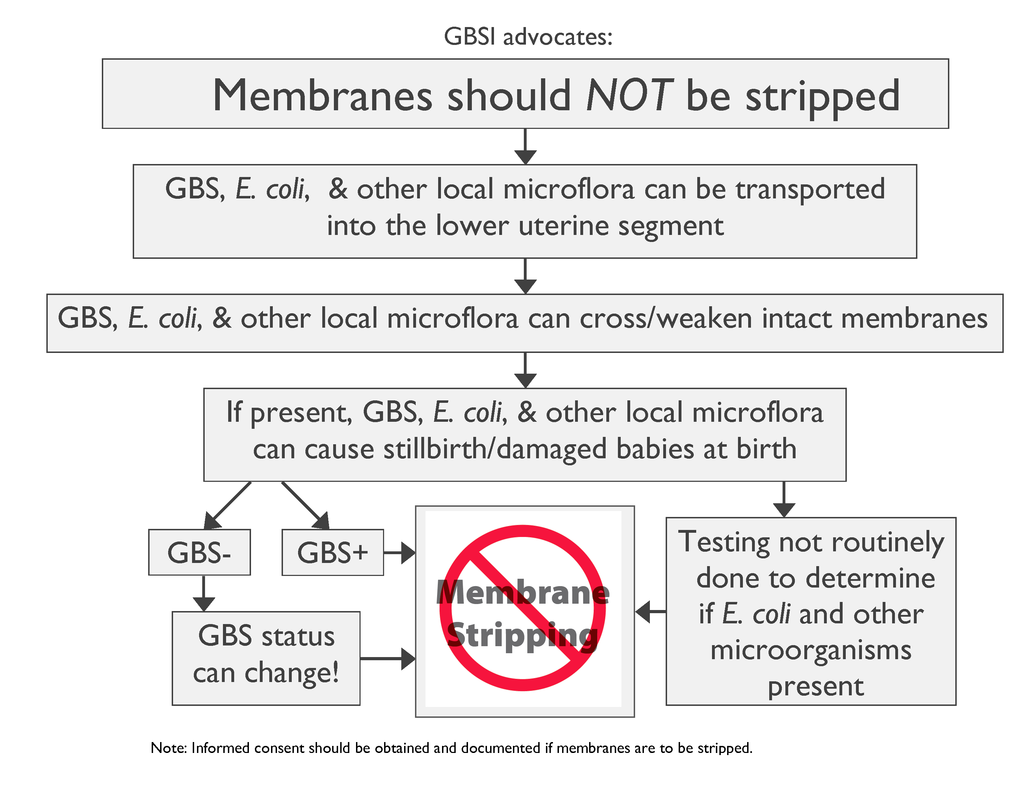
Invasive procedures may push GBS closer to your baby where GBS is able to cross intact membranes. Knowing how far you are dilated does not accurately predict when your baby will be born. Vaginal or perineal ultrasounds are less invasive options for internal exams although may not be readily available in all health care settings.
In the US, this is usually done at the first prenatal visit and is different than the standard prenatal urine “dipstick” check. The American College of Obstetricians and Gynecologists (ACOG) issued new guidance in 2019 regarding Bacteriuria (GBS in urine) in regards to early-onset disease prevention. However, studies have shown that treating asymptomatic bacteriuria can reduce the risks of preterm birth. Further research is needed to see if perhaps urine culturing can also provide opportunities to reduce the risk of GBS infection for unborn babies.
Urine culturing is important because having GBS in your urine means that you are likely to be heavily colonized vaginally where GBS could potentially harm your baby. You may have GBS in your urine without having any symptoms, but see your provider promptly if you do have any symptoms of a bladder (urinary tract) infection.
Ask about the results of your urine culture:
- If you have a significant level of GBS in your urine or any symptoms, your provider should prescribe oral antibiotics at the time of diagnosis. GBSI advocates a recheck (“test of cure”) one month after treatment.
- If you have any reportable amount of GBS in your urine, you should receive IV antibiotics for GBS during labor and delivery regardless of any future GBS test results in this pregnancy.
2) See your provider promptly for an exam if you have any “vaginitis” symptoms
GBS can cause vaginitis symptoms such as:
- external vaginal burning
- external vaginal irritation
- unusual discharge
These symptoms may be mistaken for a yeast infection and treated incorrectly.
Healthcare providers: Please view the poster presentation, Revisiting group B strep (GBS) symptomatic vaginitis (GBSSV), for more information.
View studies about Vaginitis & GBS
3) Avoid unnecessary invasive procedures
Invasive procedures may push GBS closer to your baby where GBS is able to cross intact membranes. Knowing how far you are dilated does not accurately predict when your baby will be born. Vaginal or perineal ultrasounds are less invasive options for internal exams although may not be readily available in all health care settings.
In the 201o CDC MMWR, on pg 7, the CDC discusses GBS and its ability to cross intact amniotic membranes. | “GBSI’s Information Statement on Fetal Membrane Stripping” (en español) (en français) explains why membrane stripping (or “sweeping”) should be avoided. |
“Do Not Strip Membranes in the Presence of Group B Strep and Here’s Why” by Dr. James A. McGregor. This video contains ultrasound footage illustrating active uterine transport in both a non-pregnant and pregnant patient. Video testimonials by providers as to why they avoid stripping membranes: |
GBSI’s advocacy poster “Membranes should NOT be stripped” below (en español) explains why membranes should NOT be stripped even if a woman tests negative for GBS! It is important to know that E. coli and other local microflora can also cross/weaken intact membranes.
GBSI advocates for informed consent prior to membrane stripping. Click HERE for our sample Learning Consent Form |
4) Know the signs of infection in unborn babies! Reasons to contact your provider immediately:
| The following presentation is from GBSI's 1st Annual Virtual Symposium on Prenatal-onset Group B Strep Disease. Monitoring fetal movement in the third trimester Joy Bryant, RN-C, BSN, MSN, EdD |
5) Know the warning signs and symptoms of preterm labor. GBS can cause preterm labor as well as cause a woman's water to break too soon, also known as preterm premature rupture of membranes (PPROM). According to a study in 2015, 3,500,000 preterm births may be attributable to GBS each year. Being born too soon can cause lifelong health challenges for a baby. Call your health care provider right away if you experience any of the following:
| The following presentation is from GBSI's 1st Annual Virtual Symposium on Prenatal-onset Group B Strep Disease. GBS as a Cause of Preterm Labor & (P)PROM David M. Aronoff, MD, FIDSA, FAAM |
This presentation is from GBSI's 1st Annual Virtual Symposium on Prenatal-onset Group B Strep Disease.
What Can We Currently Do to Help Prevent Prenatal-onset Group B Strep Disease? Marti Perhach Executive Director |
Learn more about the many types of prenatal infections and how to help prevent them!
JOIN THE CAMPAIGN AGAINST GBS DISEASE IN BABIES! | CONNECT TO GBSI |






















0 Comments
if you have any issue let me know plz